
The Hennepin County Mental Health Center is part of Hennepin County’s Human Services and Public Health Department, one of Hennepin Health’s four partner organizations. Because of the high rate of mental health conditions in the Hennepin Health population, the center plays an important role.
Located on the second and third floors of the Nicollet Exchange Building at 1801 Nicollet Avenue, the Mental Health Center offers a range of services, including:
- Diagnostic assessments
- Psychiatric evaluations
- Psychological evaluations
- Individual and group therapy
- Medication management
- Dual-diagnosis programs (for co-occurring mental illness and substance use disorders)
- Outreach to persons who are homeless
- Consultation
Sally Kratz and Amber Morgan
Sally Kratz, MSW, LICSW, administrative manager, and Amber Morgan, R.N., clinical care coordinator, are two staff members at the center.
Morgan joined the center in 2013 under a UCare grant. When the grant expired in March 2014, Hennepin Health began funding Morgan’s care coordination services via a 2014 reinvestment initiative.
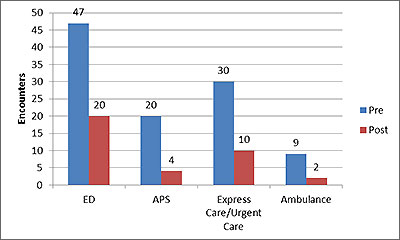
Morgan’s work appears to be having an effect. In late 2013, Dana Soderlund, MPH, Hennepin Health data analyst, looked at the pre- and post-medical utilization rates of 56 Hennepin Health members who had received Morgan’s care coordination services. Soderlund determined that the total number of emergency department (ED), acute psychiatric services (APS), urgent care, and ambulance encounters within the cohort declined after Morgan’s engagement. This chart depicts the decline:
Kratz, who has worked at the Mental Health Center since 1999, has seen the benefits of Hennepin Health’s integrated care model. As a long-time clinician treating persons with severe psychiatric disorders, she believes that traditional models of care have been inadequate and unresponsive to the many and varied client needs for individualized mental health services, primary and dental care, and social services. For Kratz, having the opportunity to participate in the planning and implementation of care coordination at the Mental Health Center has been both challenging and rewarding.
The center hopes to build on the success of care coordination services and further develop and sustain innovative approaches to service delivery.
Charles
One Mental Health Center patient is 46-year-old Charles, a Hennepin Health member who was incarcerated for 26 years (from age 18 to 44) in Saint Louis, Missouri. Although Charles doesn’t excuse the actions that led to his incarceration, he notes that his early life experiences — including a physically abusive stepfather — informed some of his choices.
Before, during, and after his release, Charles struggled with a host of mental health and chemical dependency issues including depression, anxiety, antisocial personality disorder, post-traumatic stress disorder, and alcoholism. The experience prompted him to relocate to Minneapolis in 2012; Charles believes that Minnesota’s behavioral health infrastructure is superior to many states.
From August 2012 to March 2013, Charles lived at House of Charity in Minneapolis. Here, an advocate connected him with Hennepin Health and the Hennepin County Mental Health Center.
Since he started visiting the Mental Health Center, Charles has interacted with a range of behavioral health providers, including Dr. Ngozi Wamuo, a psychiatrist; Mary Shannon-Myer, a therapist; and Amber Morgan. First, he began taking medications to help manage his symptoms and worked with Shannon-Myer to identify and address obstacles to progress. Then Shannon-Myer introduced Charles to Morgan for care coordination.
Morgan helps Charles set up his medical and dental appointments. She is also a skilled listener, someone Charles can talk to “without being judged.” Morgan introduced Charles to Connections — a men’s treatment group that meets on Tuesdays and Fridays — that she helps facilitate. Initially, Charles was resistant to Connections because he was uncomfortable with sharing his story in a group. Once he started attending, however, Amber and the members won him over with their lack of judgment. Today, he credits this willingness to share his feelings and experiences — instead of bottling them up — as key to his recovery.
One of Charles’ most memorable moments in Connections occurred during his second meeting, when a man in the group — who, Charles says, bore a striking resemblance to his biological father — told Charles that, “The greatest thing a person in our position can do” is be compliant with their medications. At the time, Charles did not take his medications consistently — in part, because he worried about their side effects. However, the man’s statement inspired Charles to “create a regimen” around taking his six prescriptions.
Charles has also found the Mental Health Center’s weekly Mental Illness Chemical Dependency (MICD) treatment group helpful. A person with long-time alcohol dependence, Charles traces his substance abuse to his stepfather; after being physically abused, he explains that he began to use alcohol as a way to “abuse myself,” and as a coping mechanism.
One Thursday in February 2014, Charles was on the number 18 bus, enroute to the MICD treatment group, when he had a moment of weakness. He explains that he rode past the center and got off downtown at Nicollet Mall. He bought a pack of cigarettes at a drug store, and was about to buy alcohol next, when he had a moment of clarity and remembers thinking, “The liquor store has nothing to do with my life right now.”
He got back on the bus and returned to the Mental Health Center.
Today, Charles describes himself as “stable” and mostly sober, but still prone to occasional bouts of depression, anxiety, and post-traumatic stress disorder. He believes that one of his greatest accomplishments is the confidence he’s gained in his ability to follow through. Kratz calls this confidence “emotional muscle.” Charles identifies it as the thing that prompted him to get back on the bus and return to the Mental Health Center, the thing that compels him to take his medications each day.
A few months ago, St. Stephen’s Human Services invited Charles to speak to a group of women about his life story. Charles was well received, and the experience made him realize that opening up could be beneficial not only to himself, but to others. “I have a lot to give,” he notes. “If [sharing my story] could deter one young man from getting in trouble or going to prison, then I’ve succeeded.”
On May 1, Charles accomplished one of his goals — he moved into his own apartment, a one-bedroom near Lake Calhoun that staff at St. Stephen’s helped him find. Other goals include remaining sober, banishing negativity, and continuing to learn how to “function in society.” Charles believes that it’s important to set realistic goals and to take things a step at a time.
“I can’t think about the future until I think about today,” he says.
Looking ahead
Kratz and Morgan are optimistic about the future of behavioral health care in Minnesota. Here are four trends they’ve noticed:
- Increased recognition of psychiatric illness as a public health issue; it affects more than the individual
- Increased acknowledgement that integrating medical, mental health, and social needs is effective
- Increased recognition that poverty is a barrier; it’s difficult to focus on recovery when you’re thinking about survival and basic needs
- Less stigma attached to mental health issues
Mental Health Center location, contact information, and hours
Nicollet Exchange Building
1801 Nicollet Avenue
2nd and 3rd floors
Minneapolis, MN 55403
General information: 612-596-9438
Appointments: 612-596-9438
Fax: 612-879-3824
Monday, Tuesday, Thursday, and Friday: 8 a.m. to 5 p.m.
Wednesday: 8 a.m. to 6 p.m.
Article appeared in the May 2014 Hennepin Health newsletter and is available here.

